The Global Toll of Preventable Cardiovascular Disease: Why Does It Matter?

“Suffering isn't ennobling, recovery is”
Christiaan Barnard, South African cardiac surgeon who performed the world's first human-to-human heart transplant operation on 3 December 1967
Sudden and unexpected, often appearing without previous symptoms or warnings, are terms that appropriately describe the utter shock that some of us feel when we learn after a relatively non-invasive angiogram test that we have a severe artery blockage that put us at high risk of suffering a deadly heart attack or stroke if no immediate action is taken. Similar reactions occur when a family member experiences a brain hemorrhage of an unknown cause, or friends or respected public figures collapse from a massive heart attack, ending their lives.
And, according to research findings, the irony involving these somber, often tragic events, that seem to come “out-of-nowhere”, is that they tend to occur more often during the holiday season, when risks are heightened due to extra disruptions to routines, diet, and sleep.
While such cardiac events are difficult to accept as a normal occurrence in the cycle of life, a new report in the Journal of the American College of Cardiology, based on the Institute of Health Metrics and Evaluation (IHME)’s Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study that has tracked trends in death and disability since 1990, shows that cardiovascular disease (CVD) continues to be the leading cause of death across the world.
A summary of the main findings of this report, complemented with information from other sources, is presented below to clearly illustrate the magnitude of this health burden that has a major impact on the quality of people’s lives, the health care system, and society as a whole.
Cardiovascular Deaths by Cause
- Overall, noncommunicable diseases (NCDs) accounted in 2019 for 7 of the world’s top 10 causes of death, according to the World Health Organization (WHO)’s 2019 Global Health Estimates. This is an increase from 4 of the 10 leading causes in 2000.
- An estimated 17.9 million people died from cardiovascular disease in 2019, representing 32 percent of all global deaths. Of these deaths, 85 percent were due to heart attack and stroke.
- Heart disease has remained the leading cause of death at the global level for the last 20 years. However, it is now killing more people than ever before. The number of deaths from heart disease increased by more than 2 million since 2000, to nearly 9 million in 2019. Heart disease now represents 16 percent of total deaths from all causes.
- The data from WHO show that about three-quarters of CVD-related deaths happen in low- and middle-income countries. This is mainly because people in these countries usually do not have the same access to primary health care programs as in the developed world. This makes the early detection and treatment of people with risk factors for CVD all the more challenging. Hence, due to the late detection, many people die at a young age from CVD, during their most productive years, further eroding the human capital of countries.
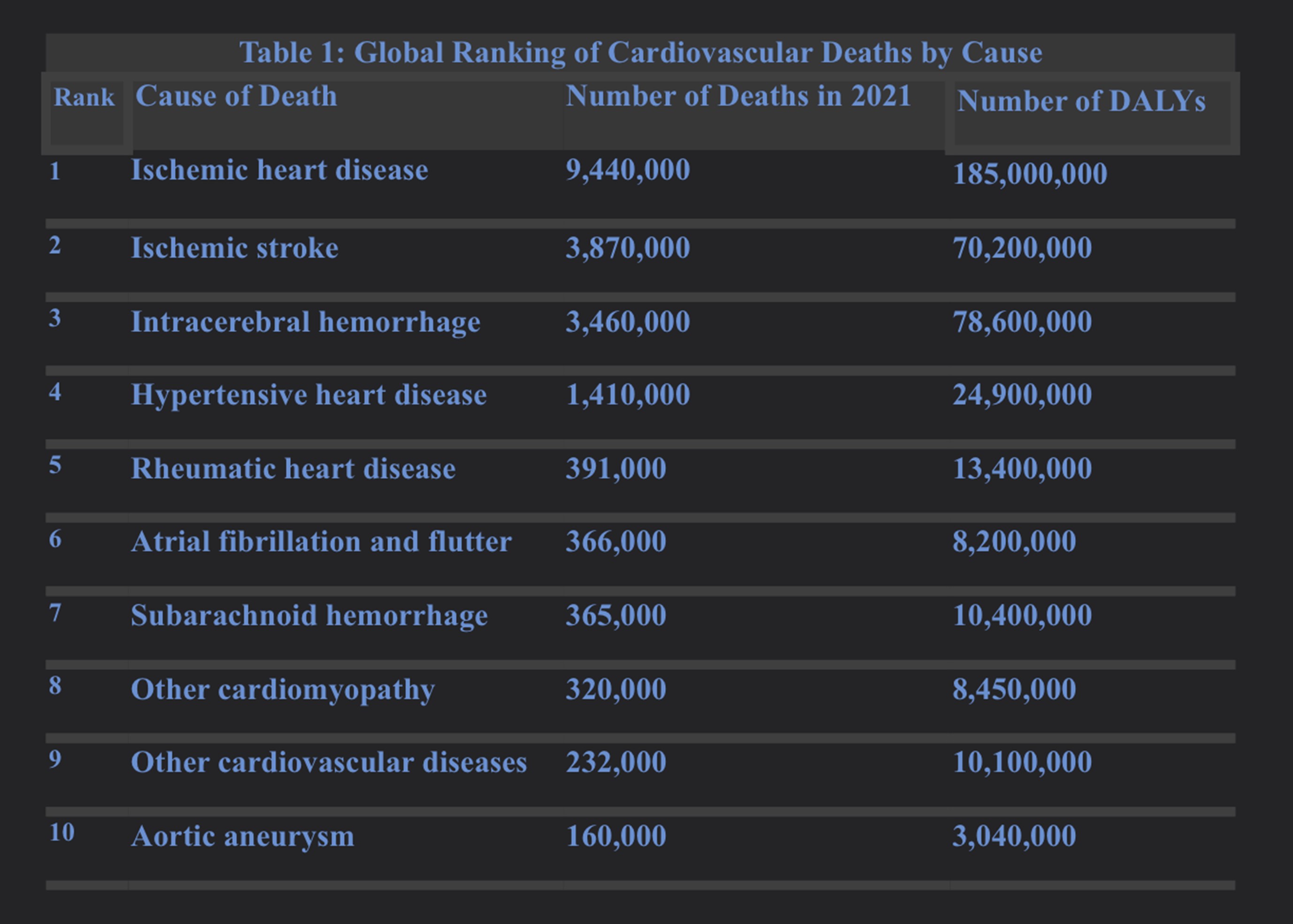
Table 1 presents the global ranking of CVD deaths by cause as of 2021 as presented in the report. The leading conditions are:
- Ischemic heart disease, or heart disease that reduces the flow of blood and oxygen to the heart, is the leading cause of cardiovascular death, accounting for 9.44 million deaths in 2021 and 185 million Disability-Adjusted Life Years (DALYs; the sum of years of life lost due to premature mortality and years lived with disability).
- Ischemic stroke, intracerebral hemorrhage, hypertensive heart disease, rheumatic heart disease, atrial fibrillation and flutter, subarachnoid hemorrhage, other cardiomyopathy, other cardiovascular diseases, and aortic aneurysm follow as the second to the tenth leading causes of cardiovascular death.
- It is estimated that over 80 percent of cardiovascular disease is preventable by addressing behavioral risk factors such as tobacco use, unhealthy diet and obesity, physical inactivity, and harmful use of alcohol.
Source: Adapted from Vaduganathan M, Mensah G, Turco J, et al. The Global Burden of Cardiovascular Diseases and Risk. J Am Coll Cardiol. 2022 Dec, 80 (25) 2361–2371.
Leading Causes of CVD
As highlighted in the report, the leading modifiable cardiovascular risk factors globally are:
---High systolic blood pressure remains the leading modifiable risk factor for premature cardiovascular deaths, accounting for 10.8 million CVD deaths and 11.3 million deaths overall in 2021. The all-cause DALYs due to high blood pressure were 2,770 per 100,000 people.
Medication helps, but controlling blood pressure with a healthy lifestyle might prevent, delay, or reduce the need for medication. It includes losing extra pounds and watching waistlines, exercising regularly, eating a diet rich in whole grains, fruits, vegetables and low-fat dairy products and low in saturated fat and cholesterol, reducing salt intake, limiting alcohol intake, quitting smoking, improving sleep quality, reducing stress, monitoring blood pressure at home, and getting regular checkups.
---Dietary risks accounted for 6.58 million CVD deaths and 8 million deaths overall in 2021. Dietary risks include food types that are under-consumed (fruits, vegetables, legumes, whole grains, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids, and polyunsaturated fatty acids) and over-consumed globally (red and processed meats, sugar-sweetened beverages, trans-fatty acids, and sodium). All-cause DALYs due to dietary risks were 2,340 per 100,000 people.
---Air pollution in the form of ambient particulate matter with an aerodynamic diameter smaller than 2.5mm (PM2.5) and household air pollution (HAP) from cooking fuels represents the leading environmental risk factor for premature CVD and mortality. In 2021, 4.75 million cardiovascular deaths and 8.54 million deaths overall were attributable to air pollution. In 2021, the all-cause DALYs due to air pollution were 2,990 per 100,000.
---Elevated low-density lipoprotein cholesterol (LDL-C) is another leading modifiable risk factor and one of the most closely linked markers of atherosclerotic CVD. In 2021, 3.81 million cardiovascular deaths and 3.81 million deaths overall were attributed to elevated LDL-C levels. In 2021, the all-cause DALYs due to high LDL-C were 1,090 per 100,000 people.
High cholesterol and triglycerides can be prevented by reducing risk factors that are under the control of people. As discussed above, healthy lifestyle decisions, such as choosing healthier foods with less saturated fat and quitting smoking, help. Medicines can also be prescribed to help lower high blood cholesterol. Statins are the most common medicine used to treat high blood cholesterol. Studies have shown that statins lower the risk of heart attack and stroke in people with high LDL-C.
---Tobacco, including smoking and secondhand smoke, is the fifth leading specific cause of cardiovascular death. In 2021, 3.01 million cardiovascular deaths and 7.61 million deaths overall were attributable to tobacco use. In 2021, the all-cause DALYs due to tobacco were 2,460 per 100,000.
Given the increased risk of CVD for smokers, cigarette smoking is one of the leading causes of preventable death that deserves priority action, particularly to prevent children and adolescents from getting hooked on tobacco early in their lives as a result of the aggressive promotion and marketing of cigarettes, e-cigarettes, and vape products. Accumulated scientific evidence shows that nicotine, a chemical in tobacco, is highly addictive, activates biological pathways that increase risk for disease, and adversely affects maternal and fetal health during pregnancy.
Smoking or chewing tobacco can also immediately raise blood pressure, albeit temporarily, as the chemicals in tobacco can damage the lining of artery walls, causing arteries to narrow, increasing blood pressure. As shown in another global study, tobacco use not only increases an individual’s risk of death from all vascular diseases two- to three-fold, but 10–30 percent of all CVD deaths are attributable to tobacco worldwide. Among men aged 30–44 years, however, 48 percent of cardiovascular deaths are attributable to tobacco use. Smokers’ risk of heart failure is twice the risk of non-smokers, and smokers with heart failure have a worse prognosis than non-smokers.
The need to confront the CVD burden globally provides the opportunity to recommit and strengthen global efforts to support countries in sharply raising taxes on tobacco products, adjusting for inflation and increased affordability due to growing incomes. Hiking up tobacco product prices and making these products unaffordable has been shown to reduce tobacco use and the health risks associated with tobacco-related diseases, including CVD. Also, tobacco-free investment is a way for investors to contribute to save millions of lives each decade, support climate action, reduce poverty, and boost development investment needed to construct a ‘new normal’ in the post-pandemic era.
---Obesity is highly prevalent worldwide, closely associated with multiple health risks, and directly contributes to the pathogenesis and progression of CVD. In 2021,1.95 million cardiovascular deaths and 3.7 million deaths overall were attributable to high body mass index (BMI). In 2021, the all-cause DALYs due to high BMI were 1,560 per 100,000.
Across the world, the most cost-effective interventions to prevent and treat obesity centers on lifestyle modification, dietary interventions, and increases in physical activity.
The implementation of these interventions is facilitated by the construction of an environment conducive to healthy behaviors, as has been shown by the Finnish North Karelia Project, that targeted cardiovascular disease risk factors, including elevated serum cholesterol, hypertension, and smoking. Through the adoption of a socio-behavioral framework utilizing community-based interventions and national-level policy changes and legislation, the project targeted lifestyle changes (e.g., minimizing the use of saturated fats and decreasing salt intake, reducing the prevalence of smoking), as a means to reduce these cardiovascular disease risk factors.
---High fasting glucose tracks closely with high burden of prediabetes, diabetes, and obesity worldwide. In 2021, 2.30 million cardiovascular deaths and 5.4 million deaths overall were attributable to elevated fasting plasma glucose. In 2021, the all-cause DALYs due to high fasting plasma glucose were 1,910 per 100,000.
Among the effective interventions to deal with this risk factor are population strategies to improve glycemic risk that overlap with approaches to other primary risk factors including low physical activity and adverse dietary profiles. In addition, continuous glucose monitoring helps to improve glycemic control, along with efforts to facilitate access to insulin, an essential treatment for many living with diabetes, as the price of insulin has increased substantially across the world in recent years, particularly in the United States.
Taxing sugar-sweetened beverages also helps to reduce consumption and prevent the onset of related chronic diseases such as cardiovascular diseases, cirrhosis of the liver, obesity, and diabetes.
Evidence reported by the World Bank consistently identifies net positive economic impacts from sugar-sweetened beverages taxes, including overall employment and productivity gains and increased government spending.
---Reduced kidney function contributed in 2021 to 1.87 million cardiovascular deaths and 3.47 million deaths. In 2021, the all-cause DALYs due to kidney function were 1,040 per 100,000.
Depending on the cause, some types of kidney disease can be treated. As people with kidney disease can have worsening high blood pressure, medications to lower your blood pressure — commonly angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers — are administered to preserve kidney function. Diuretics can help maintain the balance of fluids in the body and help relieve swelling, and administration of medications help lower cholesterol levels, treat anemia, and protect bones.
---Lead exposure remains a silent but significant contributor to CVD mortality and health loss. It is an underrecognized environmental factor that is linked with hypertension, stroke, coronary artery disease, peripheral artery disease, and other types of CVD. In 2021, 1.57 million cardiovascular deaths and 1.64 million deaths overall were attributed to environmental lead exposure. In 2021, the all-cause DALYs due to other environmental risks were 451 per 100,000.
It has been estimated that substantial decreases in environmental lead exposure may result in large population health benefits in adults. The most important step to take is to prevent lead exposure before it occurs. This can be achieved via primary and secondary lead exposure prevention. Primary prevention is the removal of lead hazards from the environment before a person is exposed to lead (e.g., eliminating lead-based paint and lead from water pipes). It is the most effective way to ensure that people do not experience harmful long-term effects of lead exposure. Secondary prevention includes blood lead testing and follow-up care and referral.
---Non-optimal ambient temperatures, an aggregate of the burden attributable to low and high temperatures, are important contributors to global mortality burdens. Although widespread attention is often paid to the mortality burden of extreme cold or hot temperatures, milder but non-optimal ambient temperatures account for far greater mortality burden. Exposure to non-optimal temperatures has been linked to cardiovascular deaths.
In 2021, 1.17 million cardiovascular deaths and 1.81 million deaths overall were estimated as attributable to non-optimal temperatures. In 2021, the all-cause DALYs due to non-optimal temperatures were 420 per 100,000.
In dealing with this risk factor, efforts in the health sector need to be fully aligned with and support climate change mitigation and adaptation actions. This is because climate change impacts a wide range of health outcomes, including CVD.
For example, as highlighted the 2022 The Lancet Countdown report, climate change, by increasing the average global temperatures and the frequency, intensity, and duration of heatwaves, raises the exposure to extreme heat which is associated with several health conditions (e.g., acute kidney injury, heatstroke, adverse pregnancy outcomes, worsened sleep patterns, impacts on mental health, worsening of underlying cardiovascular and respiratory disease, and increases in non-accidental and injury-related deaths). Exposure to extreme heat also affects health indirectly by restricting people's capacity to work and exercise, particularly impacting the elderly and other vulnerable populations.
---Low physical activity levels represent an important threat to cardiovascular health. In 2021, 0.397 million cardiovascular deaths and 0.686 million deaths overall were estimated as being attributable to inadequate physical activity. In 2021, the all-cause DALYs due to low physical activity were 193.0 per 100,000.
The evidence is clear: even small amounts of vigorous physical activity are associated with substantially lower mortality due to CVD. Recent research findings show that brief bursts of vigorous intermittent lifestyle physical activity (VILPA), that is embedded into everyday life, led among study participants to a 48-49 percent reduction in CVD mortality risk. Moreover, the sample median VILPA duration of 4.4 min per day was associated with a 26-30 percent reduction in all-cause and a 32-34 percent reduction in CVD mortality risk.
---Heavy alcohol use, especially binge drinking, defined as consuming 5 or more drinks on an occasion for men or 4 or more drinks on an occasion for women, is associated with increased blood pressure and arrhythmias. In 2021, 0.407 million cardiovascular deaths and 1.88 million deaths overall were due to high alcohol use. In 2021, the all-cause DALYs due to high alcohol use were 915 per 100,000.
As in the case of tobacco, the most cost-effective policies or “best buys” to reduce alcohol use include increasing taxes to raise the prices on alcoholic beverages, enacting and enforcing bans or comprehensive restrictions on exposure to alcohol advertising across multiple types of media, and enacting and enforcing restrictions on the retail availability of alcohol.
Other effective interventions include the enactment and enforcement of drunk-driving laws and blood alcohol concentration limits via sobriety checkpoints.
---COVID-19 has had a profound impact on health worldwide. Patients with CVD faced among the highest risks of mortality and complications when infected by COVID-19. COVID-19 may trigger acute cardiovascular events, such as myocardial infarctions or strokes, and the longer-term cardiovascular health implications of COVID-19 infection are increasingly recognized.
Also, as smoking and e-cigarette use increase the risk and severity of pulmonary infections because of damage to upper airways, lung inflammation, and reduced lung and immune function, it should not surprise us that initial evidence suggests that smoking, a leading cause of CVD, is a risk factor for COVID-19, with smokers having 1.91 times the odds of progression in COVID-19 severity compared to non-smokers. This finding is reinforced by another review showing that COVID-19 infection was associated with substantially higher severity and mortality rates in patients with chronic obstructive pulmonary disease and among current smokers.
In addition, reports of myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the outer lining of the heart) after SARS-CoV-2 messenger RNA (mRNA) vaccination have emerged. In both cases, the body’s immune system causes inflammation in response to an infection or some other trigger. Case reports, surveillance data, and other reports from the US, Israel, and Canada indicate an increased risk of myocarditis after vaccination with SARS-CoV-2mRNA vaccines, higher after the second dose, especially in younger men.
Likewise, the results of a Nordic Cohort Study of 23 million people indicated that both first and second doses of mRNA vaccines were associated with increased risk of myocarditis and pericarditis. For individuals receiving 2 doses of the same vaccine, risk of myocarditis was highest among young males (aged 16-24 years) after the second dose.
This risk, however, should be balanced against the benefits of protecting against severe COVID-19 disease and death.
The Need to Act Quickly and Effectively
The data presented above should alarm us, as the numbers are staggering. Indeed, CVD is the number 1 killer in the world, accounting for one-third of all deaths.
While IHME data show that rich countries such as the United States, Canada, Australia, New Zealand, Japan, South Korea, and others in Western Europe, have experienced steep declines in CVD mortality over the past two decades, the countries with the greatest number of cardiovascular deaths, after accounting for population size, are found in the low income and emerging economies in Eastern Europe, Central Asia, the Middle East, South America, sub-Saharan Africa, and Oceania.
The growing skewed global distribution of the CVD burden is ominous, particularly because the effective policy and institutional responses that need to be mounted stand to be undermined by a limited resource base, severe economic constraints and fiscal deficits, and underdeveloped health systems that have been overwhelmed by the COVID-19 pandemic in the past three years.
So what to do?
Waiting to treat affected individuals after the onset of CVD is not a medically efficacious nor a financially sustainable course of action, particularly in low- and middle-income countries that are struggling to implement ambitious agendas to attain universal health coverage (UHC) post-pandemic. The time has come, therefore, for a drastic paradigm shift to embrace primary and secondary prevention as critical pillars of service provision under UHC. Indeed, health promotion and disease prevention are not less valuable or secondary to treatment for controlling the spread of CVD since both are two sides of the same coin, complementing and reinforcing each other, along a continuum of interventions.
The sustained improvement of cardiovascular health globally, therefore, will require prevention, detection, and treatment of modifiable risk factors; early identification and treatment of heart attacks and strokes; and prevention of recurrent cardiovascular events. The operationalization of these actions will depend on dedicated and balanced investment in all available intervention approaches, from policy and environmental changes designed to prevent risk factors to assurance of quality care for the victims of heart disease and stroke, including improving clinical performance in emergency medical services for these conditions, monitoring the safety of medicines and vaccines, as well as communication and education to support individual efforts to prevent or control risk factors.
As we enter into a new year, 2023, let’s be guided in this endeavor, first and foremost, by the realization that CVD exacts a greater toll on global health than any other condition, often translating into early death, disability, personal and family disruption, losses of income and human capital, and increased medical care expenditures, that place individuals and families at the risk of impoverishment and bankruptcies, particularly in countries where UHC is a distant aspiration.
We should also be cognizant, as was discussed above, that this task is doable as more cumulative knowledge and experience in CVD prevention exists today than ever before.
But, we should be clear that the accumulated knowledge and experience need to be put into action now and over time through effective adoption, adaptation, and application to realize the potential public health benefit of CVD prevention across the world.
Source of Image: Stock Photo ID: 530566492