Ethics, values, and health systems: Key considerations for building back better
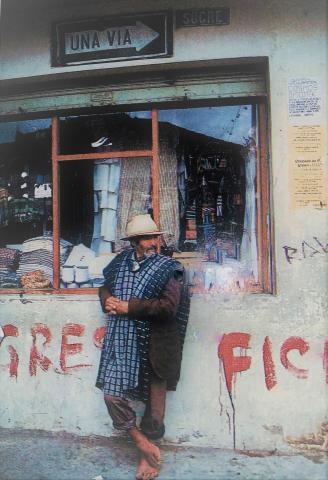
In memory of my Father, Dr. Miguel Angel Marquez (March 1934-February 2014), who believed that health for all is possible
As we start to visualize a "new normal" post-pandemic, it is important that we focus on ways to redouble our efforts to achieve universal health coverage globally. The pandemic has showed with great clarity that underfunded, institutionally weak, and hospital-centric health systems pose major public health, economic, and national security risks for all countries across the income spectrum.
While past efforts have focused on improving access to medical services and offering the population financial protection from the impoverishing impact of out-of-pocket health expenditures, limited attention has been placed on supporting the development of essential public health functions—including disease surveillance, public health laboratories for case confirmation, vital epidemiological intelligence, drug regulation, and monitoring the safety of marketed medicines and vaccines.
A course correction is therefore needed, not only to be ready to face the next epidemic or pandemic that may be lurking around the corner with the potential to cause human, social, and economic misery as severe or worse than COVID-19, but more importantly, to strengthen health promotion, disease prevention, and health protection to support the development of healthy populations, both physically and mentally, as an essential investment for building human and social capital and to enhance economic productivity and competitiveness.
If we accept that the ultimate goal of a health system, along with other social investments, is to improve the health condition of the population, then the key question that we need to pose is what kind of health system needs to be developed to achieve this goal?
To answer this question, the late Professor Uwe E. Reinhardt, distinguished Princeton University health economist, urged us to focus on broader social goals, including the distributive ethic or moral values in a country. He argued that in large measure the “structural parameters” of a health system—financing health care, risk pooling to protect individuals from the cost of illness, producing and delivering health services, purchasing or commissioning health care on behalf of patients, stewardship and governance, and production and distribution of health care resources—are determined by the shared ethic or moral values in a society.
The above consideration is of upmost importance since the economic, political, and social frameworks that each society has—its laws, institutions, and policies—result in different distribution of benefits and burdens across members of the society. These frameworks and their structures, which are the result of human political processes and are constantly changing both across societies and within societies over time, are important because the distribution of benefits and burdens resulting from them fundamentally affects people’s lives.
In the health sector, this means that alternative “distributive social ethics” or “moral values” prevalent in a society may offer three broad health care organization models to choose from: (i) a one-tier system, where health care is a social good available to all on equal terms; (ii) a two-tiered system, where health care is a social good for all with exception of the rich; and (iii) a multi-tiered system, where health care is a private consumption good like other services such as food and housing.
So, which one of these models should governments adopt, adapt, and develop post-pandemic to help build resilient and more inclusive societies? Which model should international organizations recommend as part of policy dialogue with governments moving forward? Is there an appropriate “government” versus “private market” combination that should prevail in a health system?
These questions are perhaps not very relevant for policy making or to ensure efficient allocation and use of scare resources since we may run the risk of confusing “means” with “goals”. Rather, what governments and other social stakeholders need to do first and foremost is to clearly articulate and define the overall social goals for the country over the medium and long terms. This is important, since how a health system is structured will ultimately reflect decisions on what kind of society a country wants to have.
Moving forward we have to be clear that the definition of broad social goals will ultimately guide policy and institutional decisions concerning the most appropriate and contextually relevant organizational forms, health care financing arrangements, and service delivery mechanisms that could be adopted to attain the intermediate goals of a health system (improved access, quality, efficiency, and fairness), which contribute to achievement of the ultimate goals of a health system (improved health status, financial protection, and patient satisfaction with services received).
All of us working in global health should be mindful that more than simple technocratic solutions, effective and sustainable health system reforms require not only high-level political support and predictable budgetary allocations, but clearly defined social goals that serve as a framework for developing more inclusive societies, with equality of opportunities for all, regardless of ethnic, and social backgrounds, or religious or political orientations. Indeed, if we are going to be effective in supporting health reform efforts post-pandemic, we need to see the big social and political picture and avoid getting lost in discussions and proposals that are not fully articulated or embedded in the social fabric of countries.
