How to Accelerate Universal Health Coverage in Latin America and the Caribbean?
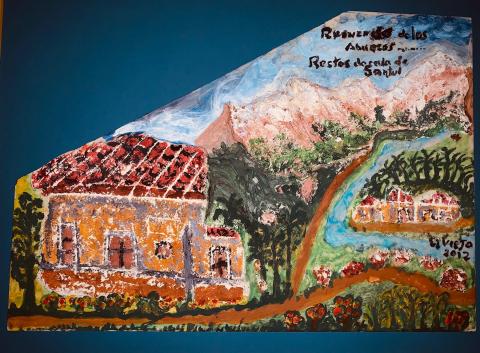
In Memory of Miguel A. Marquez, 1934-2014
Over the past four decades, major policy reforms were introduced in several Latin American and Caribbean countries to strengthen their health systems. While countries such as Brazil, Costa Rica, and Cuba managed to unify their health systems, and Chile, Colombia, and Mexico introduced organizational changes to expand health service coverage to the poorest populations as a right for all citizens, the institutional organization in most countries of the region at the beginning of the 2020 decade continues to be characterized by the coexistence of parallel subsystems that respond to the needs of different social groups in an often uncoordinated and fragmented manner. In spite of the regional heterogeneity, this segmented model of heath care organization in most countries of the region segregates different population groups according to employment and socioeconomic status into three broad institutional arrangements for accessing health services: the ministry of health, the social security institute (s), and the private sector.
Why does this matter? In 2014, PAHO/WHO Member States approved the Strategy for Universal Access to Health and Universal Health Coverage (UHC). The strategy emphasizes the need to strengthen health systems to achieve universal access and coverage, namely by reducing health inequities; expanding access to comprehensive, quality care; and improving the health and well-being of the population. The progressive realization of the UHC strategy in the region, therefore, requires a major health system transformation to deal with the fragmentation of financing and service delivery and the differential access produced by population segregation.
In advancing the health reform process in Latin America and the Caribbean in the new 2020 decade, several factors merit consideration. I will elaborate on some of them given their importance for increasing the political feasibility of reforms as well as for ensuring their financial and institutional sustainability.
Factors to Consider
The history of health care reform in the region and elsewhere shows that technically sound proposals backed by data and evidence are a vital but not sufficient condition to effect this transformation. As public policy is an inherently political process, a clear understanding and careful but active modulation of the interrelationships among individuals, organized interest groups, and governments in a given context and period of time are of critical importance to influence the design and enactment of policies, laws, and regulations that shape a health system. This implies that reform proposals in the health sector first and foremost need to clearly articulate how they will contribute to the achievement of broader social goals in a country, or more broadly stated, to construct societies that are more inclusive, where health care is a social good available to all on equal terms, rather than a private consumption good like other services such as food and housing, that is only fully afforded to the rich. The unification of vision and social goals as the frame of reference for health reform proposals is key to align the interests of different actors and mobilize their support for their adoption and sustainable implementation over time.
Indeed, as Professor Uwe E. Reinhardt, the distinguished late Princeton University health economist observed, having a clear understanding of “what kind of a society a country wants to have”, will ultimately guide policy and institutional decisions concerning the most appropriate and contextually relevant organizational forms, health care financing arrangements, and service delivery mechanisms that could be adopted to attain the intermediate goals of a health system (improved access, quality, efficiency, and fairness), which would in turn contribute to achievement of the ultimate goals of a health system (improved health status, financial protection, and patient satisfaction with health care received).
The codification into laws of health as a right of citizenry is a vital step that is required to transform health systems as it helps to translate specific policy proposals into legal mandates, institutionalizing a framework that ensures the directionality and continuity of the reform process across political cycles and helps withstand recurring bouts of political opposition and changed social and economic interests in a country.
Recent examples in the Americas offer good lessons on the interplay of policy formulation and advocacy and the sobering reality of the political processes needed for their approval and enactment that have reshaped health care organization and financing, service delivery modalities, and expanded population coverage:
Colombia, with the adoption of Law 100 in the mid-1990s, that introduced a universal health insurance program, which was amended in 2008 per the decision of the Constitutional Court that directed the Government to unify its contributory and subsidized insurance schemes; the 2003 approval by the Mexican Congress of revisions to the General Health Law that established the System of Social Protection in Health, with Seguro Popular expanding health insurance coverage to about half of the country’s population; and the Patient Protection and Affordable Care Act adopted in the United States in 2010. In previous decades, health as a human right and citizens’ entitlement were codified in the Constitutions of countries such as Cuba, after the 1959 revolution; Costa Rica in the 1960s; Brazil in the Constitution adopted in 1988; in Peru in 2002, with the introduction of the Comprehensive Health Insurance for poor and uninsured populations; and in Chile, with the adoption in 2005 of the Health Guarantees Law that introduced enforceable rights to health services for a set of diseases.
Dealing with inequitable financing, particularly needed to realize the promise of timely access to medical care when needed and to reduce out-of-pocket expenditures that create risks for catastrophic and impoverishing spending among the poor and underserved populations, is of upmost importance. Recent estimates show that out-of-pocket expenditures stood at 33 percent in 2014 and 28 percent in 2016 of total health spending on average in several countries; this level is far higher than the OECD countries average of 18 percent. This figures not only convey the stress households face in accessing health care, but acquires added relevance when one considers that among the world’s regions, Latin America and the Caribbean has one of the highest levels of social and health inequity, especially in terms of inequality in income distribution. Although income inequality has decreased over the past 15 years, in 2017, the Gini index (the most common measure of inequality; a higher Gini index indicates greater inequality, with high income individuals receiving much larger percentages of the total income of the population) stood at 0.51, the highest in the world. If, as envisioned, the targets for UHC and the health- and poverty-related Sustainable Development Goals (SDGs) are to be achieved by 2030, a sustained effort of domestic resource mobilization and increase in the relative allocation for health in national budgets is required.
Given the middle-income status of most countries in Latin America and the Caribbean, this effort, as outlined in a recent World Bank Group report for the G20, would mean in practice that as part of fiscal consolidation initiatives, governments would need to increase overall government revenue as a share of GDP, and where feasible, some of which can flow to expand fiscal space for health. To this end, there is an arsenal of measures to consider: improvements in tax administration; expansion of tax bases by increasing the range and level of taxes and charges; removal, although political difficult, of ineffective subsidies (e.g., on fossil fuel) that disproportionately benefit the non-poor; raising taxes on tobacco products and other health-damaging products, such as alcohol and sugary drinks, which not only help to reduce health risks but also are more politically acceptable to the general population than other taxes in spite of likely opposition from powerful interest groups; and reduction of the reliance on wage-based deductions or voluntary forms of insurance to bolster prepaid and pooled funding.
Leveraging health-related investments in other sectors—including, for example, in transport to reduce road traffic injuries and fatalities that impose a heavy burden on costly trauma care, in safe water and basic sanitation to reduce the risk of gastrointestinal diseases and chronic malnutrition—would improve population health, reducing need, demand and utilization of health services.
While additional funds for health would help, an equally important task is to improve the efficiency of resource use in the region. For example, a recent report suggested that 20 percent of all health expenditures in OECD countries was wasted and did not contribute to the desired health outcomes; in some Latin American and Caribbean countries, this figure may be higher. As suggested in the World Bank Group report, improvements in performance-informed planning and budgeting, enhanced budget execution, and stronger systems of public financial management in the health system would help.
Also, better allocation of existing resources is needed in order to prioritize the delivery of cost-effective primary and community health services with appropriate referral systems, away from hospital-centric models of care, and strengthen public health functions, particularly disease surveillance, public health labs for case confirmation, and epidemiological intelligence capacity, to anticipate and control societal-wide health risks associated with the reemergence of infectious diseases and the emergence of new pathogens that cross borders and threatening loss of life, economic disruption, and costs to health systems.
In the face of rapid demographic and health changes in Latin America and the Caribbean, particularly the aging of the population and the increase in the relative importance of chronic non-communicable diseases and injuries, as well as mental and substance use disorders, another priority area that merits attention for reforming health systems in the region is the need to support a fundamental rethinking of how to best keep people healthy and out of hospitals.
For starters, there has to be a widespread realization among policymakers, employers, health insurers, service providers, and the population at large, that the lion’s share of health care expenditures goes for treating diseases and injuries that could be “prevented”.
The realization of health promotion and disease and injury prevention would require supporting population-wide efforts to tackle social, environmental and behavioral determinants of ill health, premature mortality, and disability, such as fiscal and regulatory policies to curb tobacco use, second hand smoke, alcohol and substance abuse, obesity, Type-2 diabetes, road traffic injuries, and in some countries, gun violence. Insurance arrangements and health care organization and payment innovations could also be used to advance this public health agenda. For example, insurance companies, by charging lower premiums for those who quit smoking, lose weight, and pass screening tests for artery-clogging cholesterol, high blood pressure, and high sugar levels, provide an incentive for individuals and families to assume responsibility for their health.
Moving forward
Throughout the world there is an ongoing search for new and innovative ways to address health system shortcomings to better respond to present and future health challenges. Latin American and the Caribbean countries are not an exception. Reforming long-entrenched health care organization and financing arrangements is not an easy task that can be completed in the short-term.
Moving from policy intention toward the achievement of UHC as a broad development and social goal will require political commitment at the highest political level and the buy-in and active involvement of individuals, organized interest groups, and governments over the medium- and long-terms. Well informed and inclusive political strategies and sound technical proposals would help pave the way for implementing needed health system changes over the medium- and long-terms to eliminate social stratification in accessing and funding health services, build more inclusive and resilient societies, and support the development of healthy populations in the region. Opposition from interest groups and backpeddling by governments, however, should be expected as an ever-present risk that will need to be monitored and confronted during this process.

