Improving Road Safety: The Critical Role of Post-Crash Care in Saving Lives and Preventing Serious Disability
Patricio V Marquez
December 12, 2024
Traffic injuries exact a devastating toll on lives worldwide. No country is immune, as demonstrated by a recent event in my native Ecuador, where a bus collision left at least 16 people dead and 8 others injured. The increasing frequency of these events highlights the urgency of strengthening policies and interventions that ensure the safety of all road users, including pedestrians, cyclists, drivers, transit riders, and others. Everyone should have the opportunity to travel safely, regardless of their mode of transportation, while at the same time, road users share the responsibility to operate, to the best of their ability, within the expectations and boundaries of the transportation system.
The Global Burden of Traffic Injuries
In 2021, road traffic crashes (RTC) resulted in an estimated 1.19 million deaths worldwide, equating to 15 deaths per 100,000 people. Road traffic injuries (RTIs) are the leading cause of death for individuals aged 5–29 and the 12th leading cause for all ages, predominantly affecting people aged 18–59, the nucleus of human capital in a country.
Low- and middle-income countries (LMICs), which account for 60 percent of the world's vehicles, suffer 90 percent of road traffic fatalities globally. The risk of road traffic death in LMICs is three times higher than in high-income countries. Additionally, road crashes injure up to 50 million people annually globally, disproportionately affecting vulnerable road users such as pedestrians, cyclists, and motorcyclists.
Beyond the immense human suffering, traffic injuries impose heavy economic burdens, including lost household income, expensive trauma care, vehicle repairs, and insurance payouts. In LMICs, fatalities and injuries account for 2–6 percent of GDP. Also, a World Bank Group study suggests that reducing road traffic injuries in LMICs could increase GDP per capita by 7–22 percent over 24 years, underscoring the intersection of public health, road safety, and economic development.
Bridging the Gap
Proven road safety measures exist, yet many LMICs face significant challenges, including unsafe road infrastructure and cars, dangerous road user behaviors such as impaired, distracted, or drowsy driving, weak traffic laws, and poor enforcement. It should be clear, however, that even with improvements in roads, vehicles, and road users, motor vehicle crashes will still happen. A comprehensive and integrated post-crash care system can further reduce fatalities and serious injuries resulting from those crashes. The essential parts of that system include emergency communications centers, highly trained first responders and EMS personnel, emergency departments, and trauma centers.
Looking Back at my Work Experience: Improving Emergency Care in Ecuador
This topic is close to my heart. In the mid-1990s, I had the opportunity to contribute to the development of Ecuador’s emergency care system while working with the World Bank Group managing the $102 million FASBASE project (Fortalecimiento y Ampliación de los Servicios Básicos de Salud en el Ecuador). This project supported the strengthening and expansion of Ecuador’s primary healthcare system.
At the time, Ecuador lacked an organized prehospital emergency care system, relying on private vehicles or rudimentary ambulance services. Under the leadership of Dr. Alfredo Palacio, who was the Minister of Health at the time before serving as the country’s President years later, and the participation of the municipal governments and civil defense agency, the FASBASE project supported the establishment of a coordinated emergency care network in Quito, Guayaquil, and Cuenca, the three largest cities in the country, that accounted for 50 percent of emergencies. Key activities and investments included:
- Introduction of Ecuador’s First 911 System: Established in Quito and Cuenca, this system used telephone and radio communication, staffed by trained physician dispatchers to triage calls and direct Ministry of Public Health (MPH) ambulances.
- Procurement of Ambulances and Equipment: Equipped ambulances were provided to the MPH and other service providers, such as Fire Departments, Red Cross, and National Police, staffed with first-aid-trained paramedics and auxiliary personnel.
- Upgraded Emergency Care Facilities: Emergency care units in selected hospitals were refurbished, and specialized equipment was supplied.
- Protocol Development and Training: Basic and advanced life support guidelines were adopted and training that was offered to prehospital and emergency care providers.
- Monitoring System Implementation: A monitoring system was developed to track service quality and operational indicators.
These efforts helped to enhance Ecuador’s emergency care capacity, demonstrated the impact of strategic investments and partnerships, and paved the way for nation-wide expansion of service coverage in the following decades.
Learning from Global EMS Experiences
The Imperative of Timely and Effective Response
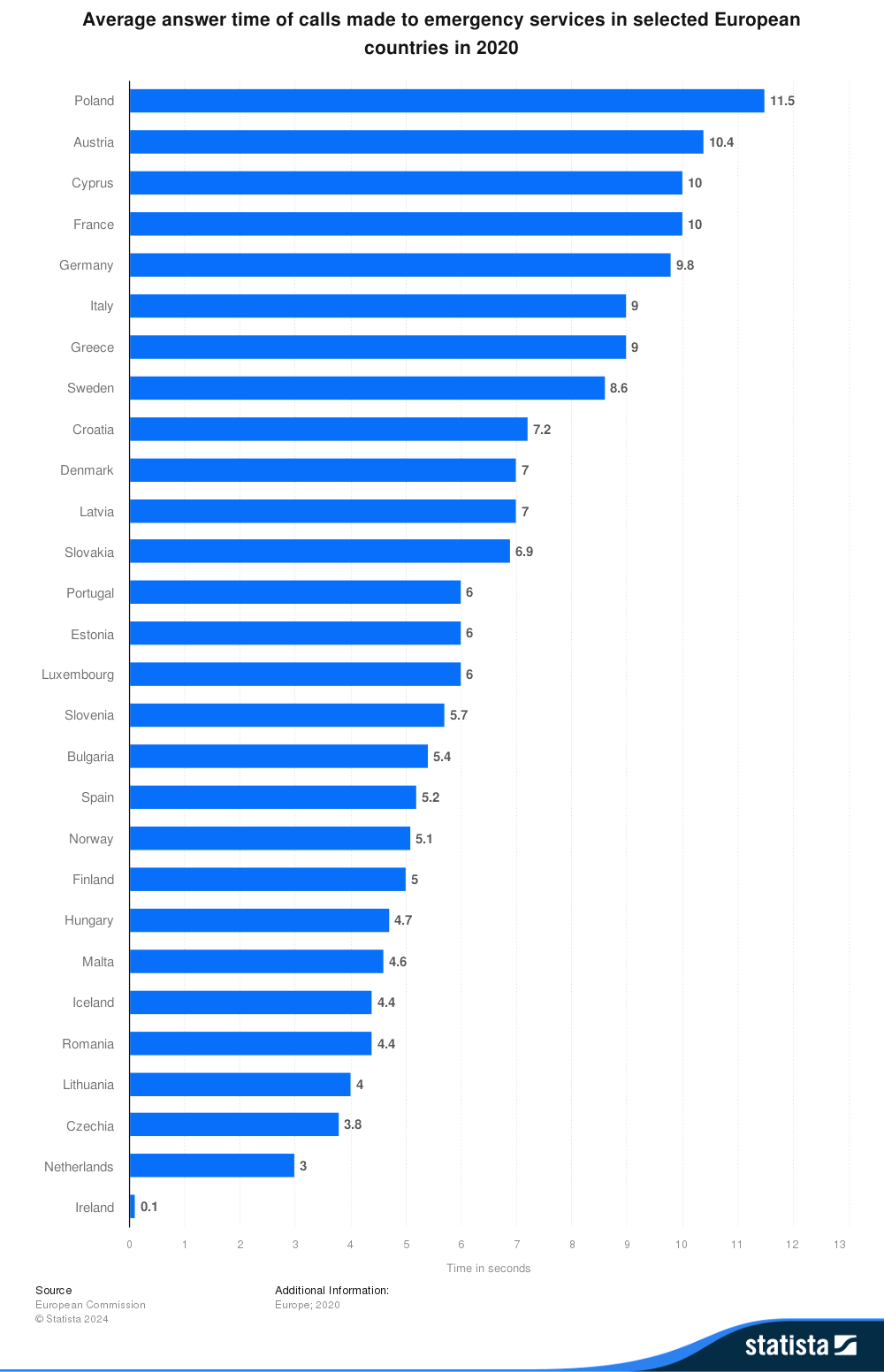
Saving lives following a motor vehicle crash depends on a well-resourced emergency care system that can provide the right care at the right time. Response time includes call handling (from the moment the call is taken by a handler to the moment an alert is raised), team dispatch (from the moment an alert is sent out to the moment a medical team is dispatched), and road time (from dispatch to arrival at the scenes). The concept of the “golden hour” emphasizes that medical intervention within the first hour of a traumatic injury is key to improving outcomes. In countries like the United Kingdom and the United States, average response times are 7–8 minutes, while as shown in Figure 1 below, European Union countries maintain times under 12 minutes. Conversely, in rural areas of LMICs, delayed responses often result in higher fatality rates. Reducing on-scene time while still ensuring adequate stabilization of the patient can strike the right balance between providing necessary initial care and facilitating rapid transport to a facility where more advanced treatment can be administered. A study on the economic value of emergency medical services highlights that reducing response time not only lowers fatalities but also improves outcomes for nonfatal cases.
Figure 1:
Leveraging Technological innovations
Technological advancements are revolutionizing emergency medical services (EMS), enabling faster response times, improved coordination, and better patient outcomes. Countries across the income spectrum are integrating new technologies to enhance both the speed and effectiveness of EMS responses. Examples include:
- Sweden: A nationwide, centralized EMS dispatch system was implemented to ensure uniform response times and quality of care. Key features include standardized protocols for dispatch and care, ensuring consistency, and GPS-enabled ambulances to optimize routes, reducing response times by 20 percent.
- India: In Tamil Nadu, the response time was dramatically improved through a dedicated call-line as well as proactive allocation and dynamic positioning of ambulances. The state also introduced triage and acuity scoring systems at the pre-hospital level to ensure prioritization of patients.
- South Korea: An AI-Ambulance initiative improved emergency care by enabling hospitals to access patient data 7 minutes before ambulance arrival, reducing treatment delays. Deployed across two cities, the system handled 3,400 cases in 2021 with 96.1% data accuracy and high diagnostic performance. AI-enhanced pre-arrival assessments allowed hospitals to prepare in advance, improving patient outcomes and saving lives.
- Rwanda: Drones deliver blood and medical supplies to remote areas, significantly cutting delays in the provision of effective emergency care. As reported by The Lancet, in the fall of 2017, Rwanda, in partnership with California-based robotics company Zipline International Inc., became the first country in the world to incorporate drone technology into its health care system for delivering blood and medical supplies to hospitals across its Southern and Western provinces. Moreover, the article noted that the world’s south, particularly Sub-Saharan Africa, lead the way in the use of medical drones and the developed world is slowly catching up.
Community Engagement
Studies underscore the importance of bystanders and first responders in emergency situations. A study in two Norwegian counties over 18 months analyzed bystander-provided first aid in trauma cases, focusing on frequency, quality, provider background, and the impact of prior training. Results showed that correct first-aid measures were provided in: Open airway: 76 percent of 43 patients; Bleeding control: 81 percent of 63 patients; and Hypothermia prevention of 62 percent of 204 patients. Those with documented training delivered higher-quality aid compared to those with unknown training status. The findings highlight the importance of first-aid training for effective responses that can save lives before the arrival of EMS.
In Singapore, EMS improvements have focused on leveraging technology and community engagement. Many of the emergency cases the Singapore Civil Defence Force (SCDF’s) team responds to could be quickly attended to by members of the public even before the arrival of the responders. The myResponder App, a mobile app alerts nearby trained volunteers to emergencies, enabling quicker first-aid administration. Average response times decreased by 4 minutes, with significant improvements in survival rates for out-of-hospital events.
Coordinated and Integrated Emergency Care Saves Lives
Besides emergency communications centers, first responders and highly trained emergency medical services personnel, access to well-resourced emergency departments and trauma centers are essential parts of post-crash care. Delays in transferring injured persons after a motor vehicle crash to a health facility when required can make the difference between life and death and lasting disability. Studies from the United States indicate that crash victims with moderate or serious injuries treated at trauma centers have a 25 percent lower risk of death.
France’s Service d’Aide Médicale Urgente (SAMU) is recognized as a global best practice in emergency medical services (EMS). Regional coordination centers (Centres 15) assess emergency calls and deploy resources using a tiered response system. Advanced life support (ALS) units, led by physicians, provide comprehensive prehospital care, including portable diagnostics and critical interventions like intubation or intravenous therapy. SAMU’s integration with the national healthcare system ensures universal access, limiting financial barriers and improving outcomes through real-time monitoring and seamless coordination.
In 2020, the National Health Commission of China issued the 'Guidance on Further Improving Pre-hospital Medical Emergency Services' to establish a nationwide three-level emergency service system by 2025 to improve pre-hospital medical care. Key goals include:
-
Developing emergency personnel and improving service capacity.
-
Expanding public first aid education and supporting related areas.
-
Establishing emergency centers with coverage of 5 km in urban and 10-20 km in rural areas.
-
Allocating one ambulance per 30,000 people, with 40 percent as negative pressure ambulances.
-
Ensuring 120 emergency calls are answered within 10 seconds and dispatched within 3 minutes.
-
Building a unified command platform and emergency training centers.
These measures aim to enhance emergency readiness and service quality across urban and rural areas. In addition, the guidance directed prefecture-level cities, eligible counties, and county-level cities to establish emergency centers or stations. Additionally, city-level emergency centers were mandated to develop training bases to equip professionals and the public with emergency skills.
Likewise, as road safety remains a pressing challenge in Latin America, with road crashes claiming approximately 150,000 lives each year, countries like Chile, Mexico, and Colombia have enacted innovative legislation in 2018, 2019, and 2022, respectively, aimed at reducing traffic injuries and fatalities. These efforts include initiatives to strengthen emergency response systems and improve trauma care for crash victims, demonstrating a comprehensive approach to tackling this public health crisis.
Colombia’s new road safety legislation of 2022, for example, aims to reduce preventable traffic deaths by improving post-crash trauma care and emergency response. Nearly half of these deaths occur at the crash scene or en route to the hospital, highlighting the need for swift and effective medical attention. To address this, the country is enhancing first responder training, upgrading ambulance equipment, and accrediting trauma centers to handle severe injuries. Medical and nursing education is also being expanded to include standardized trauma care, ensuring healthcare professionals are well-prepared. Additionally, improved data collection and analysis will identify gaps in the system and drive further improvements. By focusing on the critical "golden hour" after crashes, these measures aim to save countless lives and strengthen Colombia's emergency response infrastructure.
Ensuring the Financial Sustainability of EMS
Predicable funding is crucial for EMS sustainability. Countries have adopted a variety of funding arrangements as follows:
- United Kingdom: Funded via the National Health Service (NHS), EMS is free at the point of use and financed through general taxation.
- Australia, Canada, New Zealand and the Nordic countries are some of the other countries that rely mainly on general taxation to fund health care, including EMS. However, no country relies on general taxation alone. For example, in Canada, about 70 per cent of health spending is publicly funded though taxation, with the remaining 30 per cent largely accounted for by out-of-pocket spending (14.6 per cent) and private health insurance (12.2 per cent). Methods of levying tax vary considerably between different countries. In Sweden, for example, public funding for health care comes from both central and local taxation.
- Diversified Funding in the United States: Private insurers and Medicare/Medicaid reimburse EMS providers for emergency transports and services. Additionally, state governments have adopted innovative funding mechanisms to support EMS systems. For example, Maryland’s EMS funding comes from a mix of state, local, and volunteer sources. The Maryland Emergency Medical System Operations Fund (MEMSOF) provides annual state budget support for EMS. MEMSOF is financed through a biennial $29 surcharge on motor vehicle registrations for certain classes of vehicles, as specified in the Transportation Law. Since fiscal 2014, a $7.50 surcharge on moving violations has also contributed to the fund, along with interest earned annually on the fund balance.
- South Korea: EMS is funded by the National Health Insurance System, reducing financial barriers for citizens. Contributions collected from the insured make up the majority of financial resources (80 percent), and the remainder is covered by government subsidies funded by taxes and surcharges on cigarettes.
The effect of improving post-crash care on RTI-related mortality in LMICs
As argued in a recent The Lancet Series on road safety, there is also a strong case for strengthening trauma care in LMICs. The results of modeling conducted for the Series estimates that effective trauma systems, capable of treating all road traffic victims based on their needs, could save over 200,000 lives annually in LMICs—a 17 percent reduction in deaths. A more realistic scenario of 50 percent coverage could save over 100,000 lives per year, equivalent to an 8 percent reduction in fatalities.
Looking Ahead
Post-crash care is a critical yet often overlooked component of road safety strategies. Investing in timely emergency response, high-quality trauma care, and comprehensive rehabilitation services can significantly reduce the mortality and disability rates resulting from road traffic crashes. A holistic approach—engaging governments, healthcare providers, and communities—is essential to ensuring that crash survivors have the best chance of recovery.
When assessing the value of investing in trauma care for road safety, policymakers should also consider its broader system-wide benefits. These include improved management of other types of injuries—such as those caused by firearms, falls, and drowning—and enhanced capacity to address emergencies like cardiac arrest, ischemic heart disease, stroke, sepsis, and large-scale disasters.
As we move into the new year, 2025, we should be clear that post-crash care should be recognized as a strategic investment in building both health capital—the value of lifetime health—and human capital, which are foundational to robust economies and improved living standards. Reducing traffic injuries and fatalities is not only a public health goal but also a social imperative for fostering healthy, resilient societies and driving economic progress.
Source of image: Pictures taken by the author of Ecuador's EMS mid-1990s poster, and 911 System poster of 2017.