Social distancing in the time of COVID-19 in Latin America and the Caribbean: Costs and Benefits
Patricio V. Marquez, Santiago Herrera, and Luigi Butron Calderon
May 14, 2020
Since December 2019, following the diagnosis of the initial cases in Wuhan, Hubei Province, China, the number of the coronavirus disease (COVID-19) cases outside China increased exponentially. As of May 14, 2020, the global pandemic has resulted in over 4.4 million confirmed cases and 301,370 confirmed deaths in 188 countries/regions (Johns Hopkins University Coronavirus Resource Center & Medicine 2020). Data from WHO show that 26.4 percent of the total 1.8 million confirmed cases and 26 percent of the total 109,121 confirmed deaths in the Americas are from countries in Latin America and the Caribbean (LAC)--the bulk of confirmed cases and deaths are from the United States (WHO 2020).
Limiting face-to-face contact with others is the best way to reduce the spread of COVID-19 (CDC 2020). As such, social distancing is one of the best tools to avoid being exposed to this virus and slowing its spread locally, within countries, and across the world. People are reminded to stay at least 6 feet away from other people, not to gather in groups, stay out of crowded places, and avoid mass gatherings. Social distancing is especially important for people who are at higher risk for severe illness from COVID-19.
Contrary to what some people believe, the practice of “physical and social distancing” is not something new; it has been around for centuries as a common public health tool to control the spread of infectious pathogens into the population.
Social Distancing Measures are Centuries Old
The history of public health in LAC offers multiple examples of the use of this tool. Since colonial times, outbreaks of disease were common in these countries, largely the result of maritime trade and export of agricultural products and minerals that helped integrate the countries in this region into the world economy. The smallpox epidemic in Hispaniola (now the Dominican Republic and Haiti), registered as the first one in the colonial period, spread to neighboring islands and countries, leaving a toll of thousands of victims.
In the sixteenth and following Centuries, epidemics of different kinds made devastating sweeps across the Americas. As the spread of disease largely reflected the maritime basis for trade among the colonies, and between the colonies and mercantile powers, such as Spain and Portugal, the principles of isolation and confinement (“social distancing”) followed in Europe to control disease outbreaks were also applied in the region. In practice, beginning in Hispaniola in 1519, in accordance with the 1423 Venetian quarantine control system, measures to cope with epidemics centered on the detention of ships and the isolation of their crews and passengers outside the harbors until sufficient time had elapsed without the outbreak of “pestilences.” The latter years of the 19th Century and the early 20th Century saw various attempts by the Latin American and Caribbean countries and the United States to adopt uniform quarantine regulations at different international conferences, under the aegis of the newly established Pan American Sanitary Bureau in 1902 (now PAHO/WHO). These sought to remove barriers to steam navigation and to codify new preventive measures into specific health legislation and programs based on the great microbiological discoveries of Pasteur, Koch, and Klebs that had revolutionized public health practice in Europe.
Social Distancing in the Times of COVID-19
We should not be surprised, therefore, that in the absence of a vaccine or known therapies for COVID-19, and due to low testing capacity and ability to do contact-tracing, governments in LAC countries as elsewhere have been forced to impose once again strict social distancing measures to contain and mitigate the impact of the corona virus.
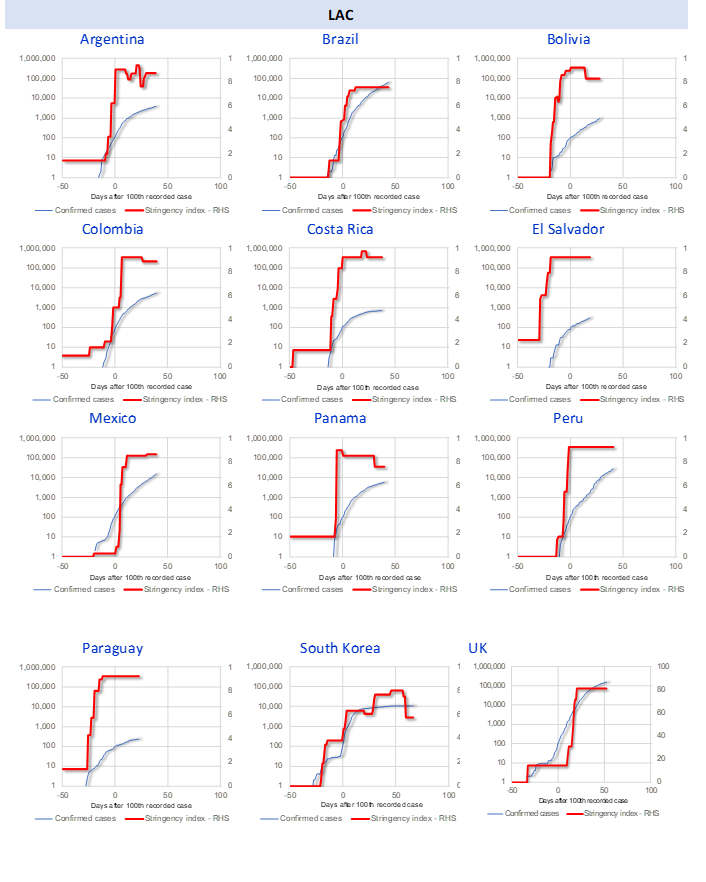
As such, the timing and severity of social distancing measures is key in containing the COVID-19 pandemic. The graphs that we have prepared below illustrate how this has happened in LAC, using the Stringency Index developed by the University of Oxford Coronavirus Government Response Tracker team, to capture variation in containment and closure policies (Petherick, Kira, Angrist, Hale, Phillips, and Webster 2020). In general, government responses have become more stringent over the course of the outbreak, and it should be expected that the stringency of response measures broadly tracks the spread of the disease. However, variation can be seen across countries. The rate at which such measures are adopted plays a critical role in stemming the infection.
In the country-specific graphs in Figure 1, the speed of the policy response is proxied by the number of days after the 100th case is confirmed (horizontal axis, with zero representing the day the 100th case was reported). In LAC, countries such as Argentina, Colombia, Costa Rica, El Salvador, and Paraguay, are good examples of preemptive policy action, while Mexico and Brazil illustrate a delayed social-distancing response. As a comparison with other regions, Figure 1 shows that South Korea’s stringency index was moving up significantly before reaching the 100th case, while the UK ramped it up after that.
Figure 1. Reported number of confirmed cases and stringency index (confirmed cases in log scale), by country
Economic Cost of the COVID-19 Pandemic
The COVID-19 pandemic is inflicting high human costs worldwide. Transmissibility and severity are the two most critical factors that determine the effect of the pandemic. Protecting lives and allowing health care systems to cope have required isolation, lockdowns, and widespread closures to slow the spread of the coronavirus. The health crisis is therefore having a severe impact on economic activity. IMF projections indicate that the global economy is expected to contract sharply by –3 percent in 2020, much worse than during the 2008–09 financial crisis (IMF 2020).
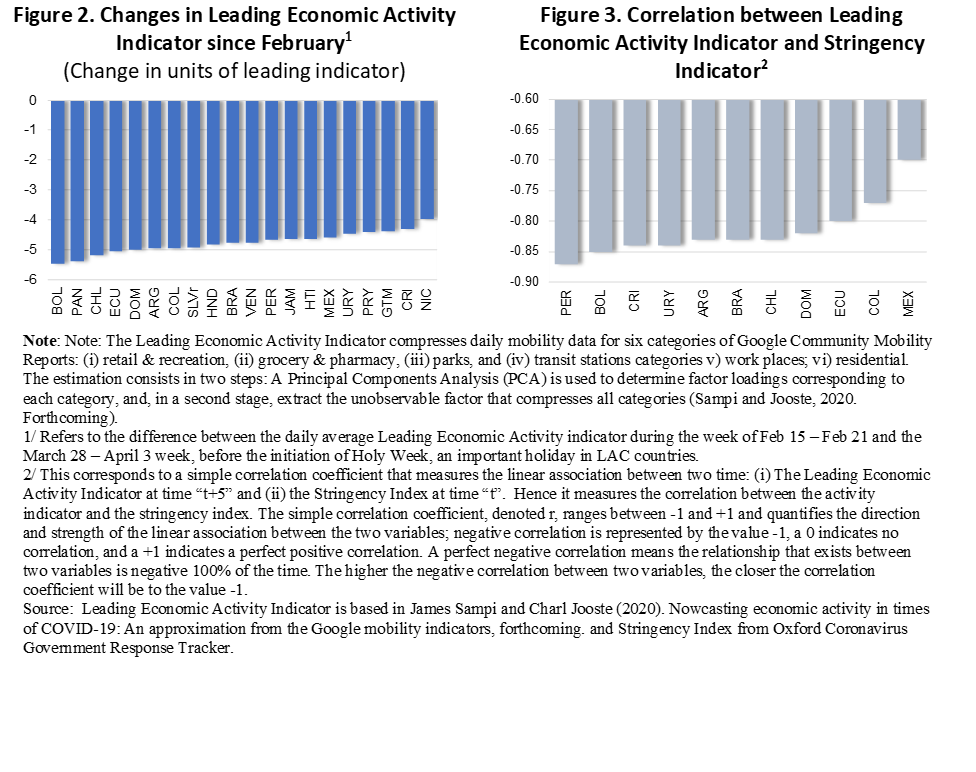
In LAC, social distancing has reduced mobility among citizens and impacted economic activity. Individual mobility is measured by Google data based on the history of cell phone locations to reveal if citizens have reduced their mobility. Using the individual mobility data as an indicator of economic activity, it can be inferred that mobility has decreased considerably across all the LAC countries listed in Figure 2 below. The combined index of Google mobility is negatively correlated with the stringency index of social distancing (i.e., the relationship between these two variables shows that as social distancing measures became more stringent, mobility decreased) (Figure 3).
Overall, economic activity in LAC is faltering. IMF projections point to severe economic slowdowns or outright contractions in LAC: a negative growth forecast for the region as a whole of –5.2 percent; with Brazil’s growth forecast at –5.3 percent and Mexico’s at –6.6 percent (IMF 2020).
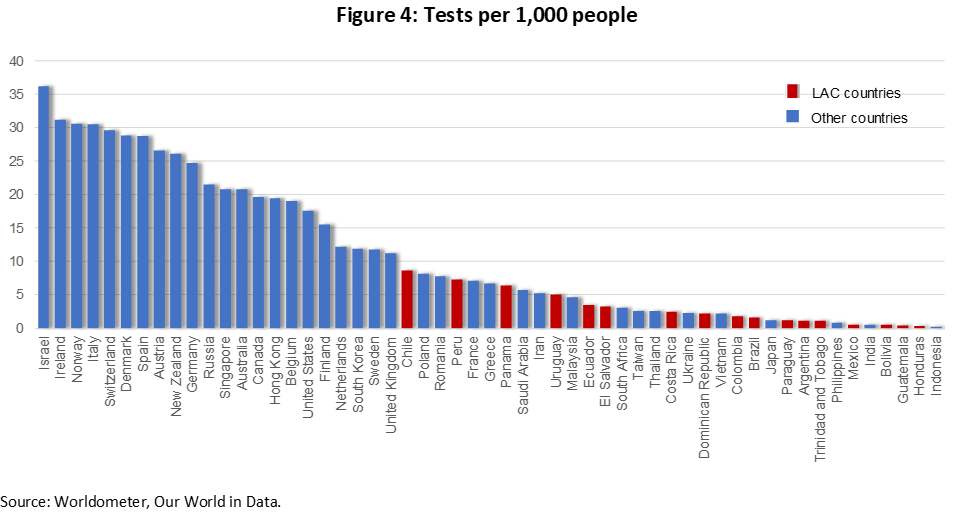
While the economic cost of the pandemic is significant, it is important to highlight that social distancing should be interpreted as the price society must pay due to imperfect information about which individuals carry the virus and the lack of adequate health care systems to manage the patient peak loads. Hence, countries that have ample testing and contact-tracing capacity as well as ample health-care facilities, can afford less restrictive social distancing. As shown in Figure 4 below, LAC countries have very low testing compared to the rest of the world, therefore, they are being forced to adopt more stringent social distancing measures. The pandemic is also hitting the region after a long economic stagnation, which led several countries to slash health care budgets, which further aggravated lack of or limited preparedness.
Excess Deaths Better Gauges the COVID-19 Toll
Although worldwide, 3.4 percent of the people confirmed as having been infected have died, WHO has been careful not to describe this figure as a case fatality rate or death rate. This is because during an evolving epidemic it can be misleading to look simply at the estimate of deaths divided by cases to date. Given the large number of asymptomatic cases, the denominator cannot be estimated without widespread testing. And there is substantial evidence that the number of deaths is underreported, as case fatality perhaps only reflects deaths in health facilities. In addition, to better gauge the pandemic’s toll, one also needs to include not only deaths from COVID-19, but also those from other causes, including people who could not be treated as hospitals became overwhelmed with patients, or those who did not seek treatment because they were afraid of being infected with the coronavirus.
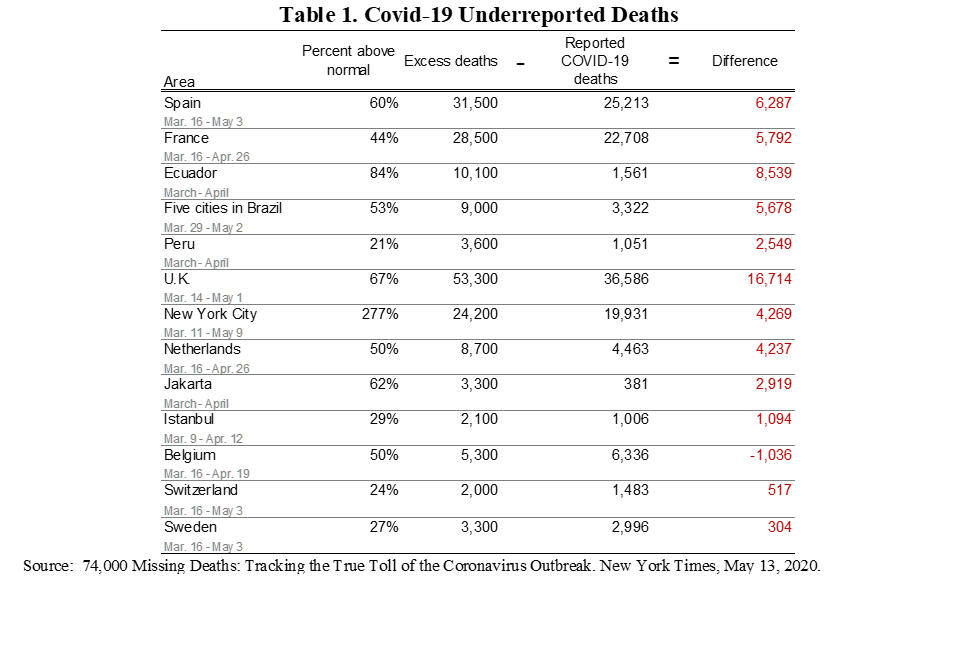
For instance, in Ecuador the number of deaths reported in the period March-April 2020 exceeded the normally reported number for those months by more than 8,000 cases, while the COVID19 reported deaths were only 1,561, suggesting significant underreporting (Table 1). In Guayaquil, a port city in Ecuador, the sudden spike in fatalities in April 2020 was comparable to what New York City experienced during its worst month: more than five times the number of people died than in previous years (Kurmanaev, Andreoni, Casado, and Taj 2020).
From an economic perspective, it should be clear that excess mortality and morbidity across population groups have the potential to undermine and reverse human capital development achieved in countries in recent decades.
Benefits of Social Distancing Measures
COVID-19 infections have been growing exponentially in many countries across the world, with the doubling time remaining between 2 and 4 days in several countries like the United States. This exponential growth is fueled by the presence of three conditions: (i) there is at least one infected person in the population pool; (ii) regular contact between infected and uninfected members of the population occurs; and (iii) there are large numbers of uninfected potential hosts among the population. Exponential growth is so powerful, not because it is necessarily fast, but because it is relentless (Siegel 2020). Without introducing a factor to suppress it, such as stringent social distancing measures, exponential growth becomes a near impossible challenge, because it doubles its presence in the population in a given amount of time.
Hence, it should be clear that while social distancing measures are disrupting economic activity, they help prevent the spread of the corona virus and save lives, tilting the cost-benefit analysis in their favor (Thunstrom, et al. 2020).
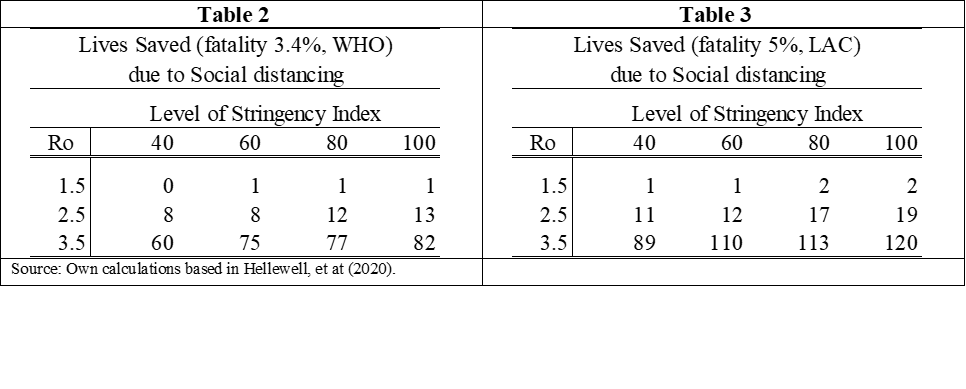
We used recent literature to estimate the impact of isolation and contact-tracing on the number of infections in the course of one month, taking into account that the number of lives saved will depend on the fatality rate that varies by country. The estimation of the number of potential infections is based on key parameter assumptions: a) the degree of contagiousness, measured by the parameter Ro; b) the extent of social isolation; c) the ability to do contact tracing, and d) the speed with which the self-isolation takes place after the symptoms manifest.
The degree of contagiousness changes over time as shown by Arroyo et al. (2020). Hence, we assume different values for the parameter, based on the LAC data. The degree of isolation can fluctuate from zero (ignorance of any restrictions) to 100% (complete isolation going out to only to purchase groceries). Using an online tool that implements the Hellwell et al. model (IFLscience 2020), we estimate the number of lives saved, based on different fatality rates, from 3.4% (cited by WHO) to 5% (a common rate in LAC). These back-of-the envelope estimations show that the benefits--the number of lives saved--increase with stringency and with assumptions of infectiousness (Tables 2 and 3).
The level of contagiousness, which changes over time (Arroyo et. al. 2020), is not completely exogenous, as it is correlated with the stringency social distancing as measured by the stringency index of the Oxford COVID-19 Government Response Tracker. There is a high negative correlation between the two independent sources of data. In fact, the purpose of the social distancing measures is to reduce the value of Ro, and the high negative correlation indicates that the measures have been effective.
What Next?
It should be clear to all that in the absence of vaccines and cures, social distancing measures are a critical tool to help suppress transmission of the coronavirus below the basic reproduction number of 1.0 (Ro), which is necessary to rapidly reduce case incidence, keep cases to low levels, and maintain that situation over time.
As warned by different international experts, if countries reopen their economies too soon without ensuring that they have in place critical testing capacity, ability to trace the contacts of those infected, and adequately prepared medical care services to deal with a surge of severe cases in the event of a resurgence, the consequences would be dire. With deaths now declining, governments are trying to restart their economies, by gradually releasing the lockdown. But, local authorities’ fear of a new outbreak is pushing back central governments’ reopening decisions--in Ecuador, for example, only two of the country’s 221 cities have moved toward relaxing the quarantine nearly a week later after the central government announced the reopening.
As observed by leading global experts, the COVID-19 pandemic is a stark remainder of the ongoing challenge of emerging and reemerging infectious diseases and the need for constant disease surveillance, prompt diagnosis, and robust research to understand the basic biology of new organisms and our susceptibilities to them, as well as to develop effective countermeasures to control them (Fauci, Lane, Clifford, and Redfield 2020).
Looking into the future, the global spread of COVID-19 clearly signals the need, hopefully once and for all, for building and maintaining strong and sustainable public health and medical institutions and systems, and an effective cross sectoral interface between environment, veterinary and public health services to anticipate, prevent, and control the emergence of new infectious pathogens of animal origin, the resurgence of known infectious diseases, and the ominous threat of anti-microbial resistance. This task is of priority importance where health systems are weaker, living conditions often more overcrowded, and populations most vulnerable. If this is not done, as the COVID-19 pandemic is demonstrating now, the risk posed by novel infectious diseases that can emerge in any part of the world at any time, causing massive social and economic disruptions, will continue to threaten the entire global community.
